28yr old patient with pain abdomen and vomitings
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Case presentation:
29 yr old male patient who is a resident of ramannapet and cashier by occupation in a petrol bunk presented to general surgery op on 21/09/2020 with complaints of pain abdomen and vomitings from three days .The case was handed over to general medicine on 23/09/2020.
HOPI-
Patient was apparently asymptomatic three days back and then he developed epigastric pain which was sudden in onset gradually progressing in severity and buring type of pain.The pain is radiating to back and it is relieved by sitting and leaning forwards.
The pain is also associated with vomitings from on the first day 12 episodes
Non Bilious type and also has food particles relieved by taking medication from the local RMP doctor {pain killers,ondansetron,digene syrup and iv fluids for two days}
The pain is not relieved by the medications so the came to our hospital.
He also complains of decreased appetite and constipation from two days
No H/O fever.
PAST HISTORY-
No H/O hypertension , diabetes mellitus , tuberculosis
No H/O previous blood transfusions or any surgeries
No H/O similar compliants in the past
PERSONAL HISTORY-
Appetite decreased
Constipation present
Mixed diet
Addictions alcoholic from four years takes whiskey quarter per day
Non smoker
GENERAL EXAMINATION -
Patient is conscious coherent co operative
Moderately built and nourished
No pallor
Icterus present
No clubbing
No cyanosis
No lymphadenopathy
No pedal edema
Geographic tongue seen
VITALS -
Patient is afebrile
BP - 130/80 mm hg sitting postion right arm
Pulse - 86bpm regular rhythm
RR - 16cycles per minute
SYSTEMIC EXAMINATION-
Per abdomen-
Inpection : Shape of the abdomen normal
No scars , sinuses ,no visible pulsations ,no visible peristalsis
Hernial sites intact
Cullen’s sign negative
Grey turner’s sign negative
Palpation : no localised rise of temperature
Tenderness at epigastric region
No organomegaly
Percussion : resonant note all over abdomen
Auscultation : bowel sounds sluggish on 23/9/2020
Bowel sounds normal on 24/9/2020
Respiratory system - bilateral air entry present
Normal vesicular breath sounds
No wheez and crepetations
CVS -S1 and S2 heard
No murmurs
CNS -No abmormality detected
INVESTIGATIONS -
21/09/2020
CBP
LFT
SERUM CREATININE
BLOOD UREA
SERUM AMYLASE
SERUM LIPASE22/09/2020
URINE FOR BILE SALTS AND BILE PIGMENTS
RBS
24/09/2020
HAEMOGRAM
LFT
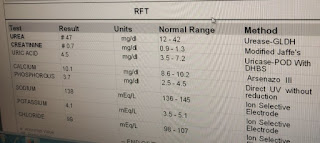
RFT
DIAGNOSIS:
ACUTE INTERSTITIAL PANCREATITIS SECONDARY TO ALCOHOL WITH MINIMAL ASCITES
BISAP SCORE 0/5 ( B-BLOOD UREA NITROGEN I-IMPAIRED MENTAL STATUS S-SIRS A-AGE P-PLEURAL EFFUSION) CT SEVERITY INDEX 6/10
TREATMENT:
NBM ON DAY 1 AND THEN SOFT DIET IS ALLOWED
IVF 1)NS 2)RL 3)DNS
INJ PAN 40mg IV OD
INJ ZOFER 4mg SOS
INJ BUSCOPAN 1amp IM STAT ON DAY1
INJ THIAMINE 100mg IV BD IN 100ml NS
INJ OPTINEURON 1amp IV BD IN 100ml NS
SYP CREMAFFIN PLUS PO 10ml
MONITOR VITALS




















Comments
Post a Comment